Not all cow’s milk is created equally. Its nutritional composition often varies slightly, depending on the cow’s breed, feed or individual genetics.
For example, cow’s milk contains varying amounts of proteins known as A1 and A2 beta-caseins. For some people, A1 beta-caseins can cause adverse health effects.
Recently, researchers examined the digestive effects of A1 beta-casein in people with self-reported lactose intolerance. Here is a detailed summary of their results.
Background
Most cow’s milk contains both A1 and A2 beta-casein, but the proportions depend on the cow’s breed. A few years ago, a New Zealand corporation started marketing A2 milk, which contains only A2 beta-casein.
This is because A1 beta-casein has been associated with adverse health conditions, such as type 1 diabetes and heart disease.
Unlike A2 beta-casein, the A1 version releases an opioid peptide known as beta-casomorphin-7 (BCM-7) during digestion.
For this reason, A1 beta-casein has been under scrutiny in recent years. However, the evidence is far from conclusive and human studies are lacking.
There is also evidence suggesting that BCM-7 may cause digestive discomfort — bloating, gas and diarrhea — resembling lactose intolerance.
One trial showed that A1 milk may cause softer stools, compared to A2 milk, and animal studies indicate that A1 beta-casein may significantly increase intestinal inflammation.
Article Reviewed
A team of researchers from China and New Zealand compared the effects of A1 and A2 milk on people with self-reported lactose intolerance.
Effects of milk containing only A2 beta casein versus milk containing both A1 and A2 beta casein proteins on gastrointestinal physiology, symptoms of discomfort, and cognitive behavior of people with self-reported intolerance to traditional cow’s milk.
Study Design
This was a randomized controlled trial comparing the health effects of A1 beta-casein and A2 beta-casein on digestive symptoms, inflammation and mental processing.
A total of 45 Chinese adults, with self-reported lactose intolerance, participated in the study. None of them regularly consumed cow’s milk.
At the start of the study, all of the participants did not drink any milk for two weeks. Afterward, they were assigned to two groups in a random order:
- A1 milk group: For two weeks, the participants consumed 8.4 oz (250 ml) of conventional milk after two meals every day. This milk contained 40% A1 beta-casein and 60% A2 beta-casein.
- A2 milk group: For two weeks, the participants consumed 8.4 oz (250 ml) of A2 milk after two meals every day. The A2 milk contained only A2 beta-casein.
Both types of milk were provided by the a2 Milk Company in New Zealand. They were identical, apart from differences in the amounts of A1 and A2 beta-casein.
The participants were told not to consume any other dairy products during the study.
The study had a crossover design, which means that all participants were in both groups on separate study periods, separated by a 2-week washout period.
At the start and end of each of the two study periods, the researchers assessed digestive symptoms and collected blood and fecal samples.
Intestinal function was measured at the end of each study period using an electronic smart pill. Additionally, all participants took a Subtle Cognitive Impairment Test.
Bottom Line: This was a randomized, crossover trial in Chinese milk-sensitive individuals. It compared the effects of conventional milk and A2 milk on digestive symptoms, inflammation and cognitive function.
Finding 1: A2 Milk Did Not Affect Digestive Symptoms
This study suggests that A2 milk doesn’t worsen self-rated digestive symptoms — bloating, flatulence and stomach rumbling — in milk-sensitive individuals.
Conversely, symptoms tended to be greater when conventional milk was consumed.
Although the difference wasn’t significant overall, symptoms were significantly greater compared to the baseline at some of the lab visits.
Since the A2 milk contained the same amount of lactose as the A1 milk, the findings strongly suggest that A1 beta-casein may be responsible for increasing symptoms.
And, even though all of the participants thought they were lactose intolerant, only 51% of them actually turned out to be intolerant to lactose.
Interestingly, lactose-intolerant individuals seemed to be unaffected by the A2 milk. It didn’t significantly worsen symptoms, even though it contained substantial amounts of lactose. The reason for this paradox is unclear.
Bottom Line: Drinking conventional milk tended to worsen digestive symptoms, even in those who weren’t lactose intolerant. These findings suggest that A1 beta-casein may be responsible for digestive discomfort.
Finding 2: A1 Milk Impaired Mental Processing
Cognitive performance was evaluated using the Subtle Cognitive Impairment Test, which measures the speed and accuracy of mental information processing.
The study found that both cognitive speed and accuracy were slightly lower after drinking the A1 milk for two weeks, compared to the A2 milk.
The authors suggest these changes may be caused by worsened systemic inflammation. Similar effects have been observed in patients with untreated celiac disease.
Some researchers have also speculated that A1 beta-casein, or its breakdown product BCM-7, may be associated with mental problems.
This is the first study to show that A1 beta-casein may affect mental processing in healthy people. Further studies need to confirm these findings.
Bottom Line: Drinking conventional milk for 2 weeks slightly impaired mental performance, compared to A2 milk, in milk-sensitive people.
Finding 3: A1 Milk Increased Inflammation
Inflammation in the stomach and small intestines was evaluated by a gastroenterologist using images taken by an electronic smart pill.
This evaluation suggested that small bowel inflammation improved in 36% of the participants when they switched from the A1 milk to the A2 milk.
Similarly, stomach inflammation improved in 23% of the participants. There were also significant differences in inflammatory markers, according to blood tests.
Specifically, levels of the inflammatory markers IL-4, IgG, IgE and IgG1 were higher after 2 weeks of drinking the A1 milk, compared to the A2 milk.
The chart below shows the estimated difference between groups (A1-A2):
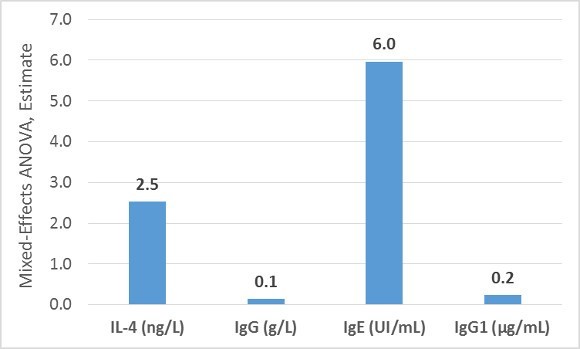
These findings are consistent with a few studies in mice showing that A1 beta-casein resulted in greater inflammatory responses in the intestinal tract.
Bottom Line: Drinking conventional milk for 2 weeks appeared to increase inflammation in the digestive tract, compared to A2 milk.
Finding 4: A1 Milk Changed Stool Form and Frequency
The participants rated their stool frequency and consistency every day using the Bristol Stool Chart. During lab visits, and at the start, middle and end of each study period, the participants also rated their digestive symptoms.
The study showed that drinking the A1 milk increased stool frequency and led to softer stools and diarrhea. Conversely, the A2 milk had no such effects.
These findings are supported by one previous study in humans linking A1 beta-casein with softer stools.
Possibly explaining these findings, the present study found that the A1 milk increased intestinal transit time, as well as intestinal inflammation.
Bottom Line: Drinking conventional milk for 2 weeks softened stools and increased stool frequency, compared to A2 milk.
Finding 5: A1 Milk Reduced Levels of Short-Chain Fatty Acids
Short-chain fatty acids are formed in the colon when beneficial bacteria ferment prebiotic fiber (17).
They reduce inflammation and are the main source of nutrition for the cells lining the colon, potentially improving colon health.
Fecal levels of short-chain fatty acids were significantly higher after drinking the A2 milk for two weeks, compared to the A1 milk. These included total short-chain fatty acids, as well as acetate and butyrate.
The estimated difference (A1-A2) in the levels of short-chain fatty acids are presented in the chart below:
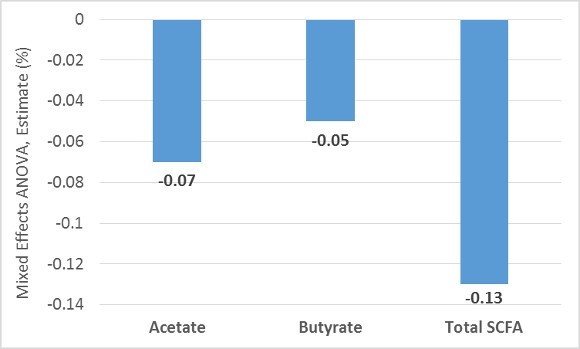
The reason why conventional milk decreases short-chain fatty acids, and A2 milk does not, is unclear.
Bottom Line: Conventional milk reduced levels of short-chain fatty acids in the colon, compared to A2 milk.
Limitations
This study had several limitations. First, all of the participants had self-reported milk sensitivity, but only half of them turned out to be lactose intolerant.
A1 beta-casein may not have any adverse effects in people who are not lactose intolerant, or otherwise sensitive to milk. Further studies need to confirm these findings in people who are not milk-sensitive.
Second, in the abstract, the researchers claim to have detected elevated circulating levels of BCM-7 after the participants had consumed A1 milk for 2 weeks.
Yet these results are not presented or discussed anywhere in the article.
Finally, one of the main authors and designers of the study was an employee of the a2 Milk Company, which holds the patent for A2 milk. The study was also solely funded by the a2 Milk Company, creating a potential conflict of interest.
Bottom Line: The results of this study may not apply to people who are not milk-sensitive. Although there is no reason to suspect misconduct, the findings should be confirmed by an independent research group.
Summary and Real-Life Application
This study found that when milk-intolerant individuals consumed A2 milk for two weeks, they experienced no significant adverse effects.
On the other hand, conventional milk containing both A2 and A1 worsened digestive symptoms. It also increased inflammation, softened stools, reduced the levels of healthy short-chain fats in the colon and slightly impaired mental performance.
Taken together, these findings suggest that milk-intolerant individuals can safely drink A2 milk, without any adverse symptoms.
However, further studies need to confirm the findings.
